1. Gregory, G. A., Kitterman, J. A., Phibbs, R. H., Tooley, W. H., & Hamilton, W. K. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N. Engl. J. Med. 284, 1333–1340 (1971).
2. Avery, M. E. et al. Is chronic lung disease in low-birth-weight infants preventable? A survey of eight centers. Pediatrics 79, 26–30 (1987).
3. Wung, J. T., Driscoll, J. M., Epstein, R. A., & Hyman, A. I. A new device for CPAP by nasal route. Crit. Care Med. 3, 76–78 (1975).
4. De Paoli, A. G. Nasal CPAP for neonates: what do we know in 2003? Arch. Dis. Child. – Fetal Neonatal Ed. 88, 168F–172 (2003).
5. Morley, C. & Davis, P. Continuous positive airway pressure: current controversies. Curr. Opin. Pediatr. 16, 141–145 (2004).
6. Sweet, D. G. et al. European consensus guidelines on the management of respiratory distress syndrome – 2019 update. Neonatology 115, 432–450 (2019).
7. Gupta, S. & Donn, S. M. Seminars in Fetal and Neonatal Medicine Continuous positive airway pressure: Physiology and comparison of devices. Semin. Fetal Neonatal Med. 21, 204–211 (2016).
8. Courtney, S. E. & Barrington, K. J. Continuous positive airway pressure and noninvasive ventilation. Clin. Perinatol. 34, 73–92, vi (2007).
9. Alessi, S. Evidence Regarding the Use of Bubble Continuous Positive Airway Pressure in the Extremely Low Birth-Weight Infant: Benefits, Challenges, and Implications for Nursing Practice. Adv. Neonatal Care 18, 199–207 (2018).
10. Martin, S., Duke, T., & Davis, P. Efficacy and safety of bubble CPAP in neonatal care in low- and middle-income countries: a systematic review. Arch. Dis. Child. Fetal Neonatal Ed. 99, F495-504 (2014).
11. Magnenant, E. et al. Dynamic behavior of respiratory system during nasal continuous positive airway pressure in spontaneously breathing premature newborn infants. Pediatr. Pulmonol. 37, 485–491 (2004).
12. Bhutani, V. K. Development of the Respiratory System. In Manual of Neonatal Respiratory Care 3–15 (Springer US, 2012). doi:10.1007/978-1-4614-2155-9_1
13. Diblasi, R. M. Nasal continuous positive airway pressure (CPAP) for the respiratory care of the newborn infant. Respir. Care 54, 1209–1235 (2009).
14. Higgins, R. D., Richter, S. E., & Davis, J. M. Nasal continuous positive airway pressure facilitates extubation of very low-birth-weight neonates. Pediatrics 88, 999–1003 (1991).
15. Finer, N. N. et al. Early CPAP versus surfactant in extremely preterm infants. N. Engl. J. Med. 362, 1970–1979 (2010).
16. Tooley, J. & Dyke, M. Randomized study of nasal continuous positive airway pressure in the preterm infant with respiratory distress syndrome. Acta Paediatr. 92, 1170–1174 (2003).
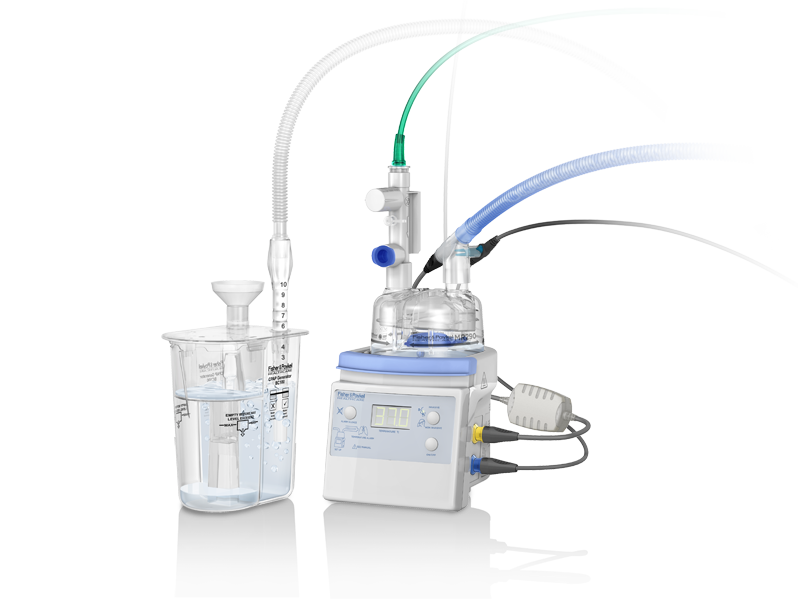
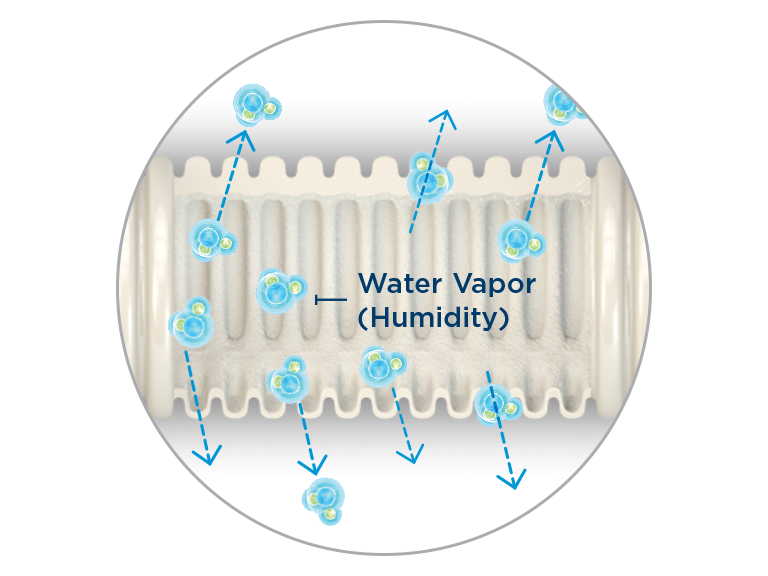
The Fisher & Paykel Healthcare Bubble CPAP generator is designed to provide consistent pressure through an auto-leveling feature. This design moves excess liquid into a separate chamber from the main pressure-generating section, automatically ensuring that the set pressure does not change with liquid build-up.
The bubble generator includes an overflow container that can be detached to remove excess water from the system, without disrupting delivery therapy.